For some years now, we have been in close contact with the anti-cancer activist Myriam von M. She started her FUCK Cancer campaign in 2014 and has been an idol for cancer patients and their relatives ever since. People who belong to the risk group for cervical cancer have also turned to Myriam von M. on Facebook. She has reached out to women with abnormal findings to share their experiences.
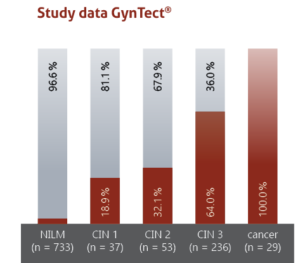
When reading the submissions we noticed that many women felt insecure or even guilty after an invasive procedure. In particular, pregnant women or women who want to have children wonder if they have done everything possible to avoid miscarriage. GynTect is an option which can respond to a patient’s unique situation.
Here is a selection of the submissions: